In Vivo Noninvasive Optical Detection of Invisible Precancer in the Human Digestive System
The purpose of this program is to develop optical systems that can perform rapid optical scanning and multispectral imaging of the entire epithelial surface of various organs in the human digestive system and present a
diagnosis in near real time. This approach should be vastly superior to the present strategies of performing random biopsies, providing a powerful tool for screening large populations of patients for early precancerous
changes. A clinically useful technique for the detection of precancer must rapidly survey a comparatively large area while simultaneously detecting changes on a cellular scale. We felt we could achieve both goals by
combining light scattering spectroscopy (LSS) with rapid optical scanning.
There are three main components of tissue light scattering spectra. The largest is a diffuse background signal from submucosal tissue; next is scattering by small organelles; and, lastly, a relatively small backscattered
component from epithelial cell nuclei. The submucosal background can be excluded by one of several gating techniques and the smaller organelles have a very different scattering spectral dependence than that of the nuclei.
Elastic light scattering can also be used to measure other cellular compartments, such as mitochondria, the spectra of which are sufficiently different from that of nuclei to be distinguished. The combination of gating
and difference in spectral behaviour allows the epithelial nuclear scattering spectrum to be isolated in the processed LSS signal. We have developed light scattering multispectral imaging instruments that use these
principles to solve the difficult problem of identifying precancerous and early cancerous in the esophagus and pancreas.
Esophageal cancer is increasing in frequency in the United States faster than any other
cancer. Barrett’s esophagus, an otherwise benign complication of esophageal reflux, affects approximately three million Americans and precedes almost all cases of esophageal cancer. If detected at the precancerous stage,
most esophageal cancers can be prevented. Standard-of-care screening for precancer uses visual endoscopy and a prescribed pattern of biopsy. This procedure, in which a tiny fraction of the affected tissue is selected
for pathological examination, has a low probability of detection because precancer is highly focal and visually indistinguishable.
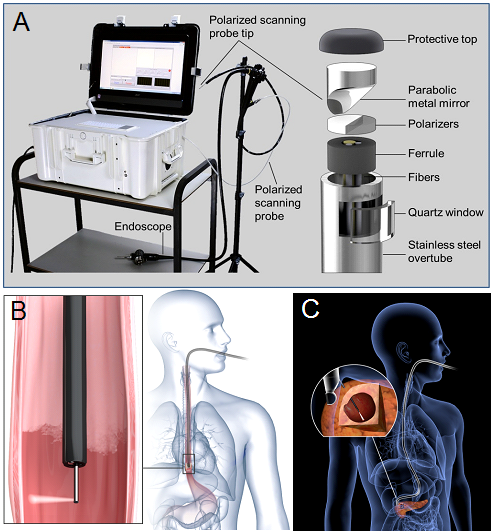
Compatible with existing endoscopes, the esophageal LSS instrument we have developed
performs rapid optical scanning and multispectral imaging of the entire esophageal surface, providing diagnoses in near real time. It is distinguished by its ability to locate precancer in tissue that shows no visible
abnormalities or lesions when observed with white light or fluorescence. By elucidating microscopic subcellular structure with macroscopic spectral measurements, the instrument locates precancerous tissue independent
of any visual cues. By detecting and mapping suspicious sites, guided biopsy of invisible precancer becomes practicable (Nature Medicine 2010,
Light Sci. Appl. 2018).
Pancreatic cancers are usually detected at an advanced stage and have poor prognosis. About one-fifth of these arise from pancreatic cystic lesions. Yet, not all lesions are
precancerous, and imaging tools lack adequate accuracy for distinguishing precancerous from benign cysts. Therefore, decisions on surgical resection usually rely on endoscopic ultrasound-guided fine-needle aspiration
(EUS-FNA). Unfortunately, cyst fluid often contains few cells, and fluid chemical analysis lacks accuracy. This can have dire consequences, including unnecessary pancreatic surgery for benign cysts and the development
of cancer.
We have developed a new LSS instrument that identifies precancerous and early cancerous lesions in the pancreas. The instrument can probe the internal surface of pancreatic cysts, obtaining multiple
noninvasive optical ‘biopsies’ from each cyst in a matter of seconds, performing significantly better than existing cytology and cyst fluid CEA markers. Our results indicate that this technology has significant
potential to aid in identifying both precursor lesions and early-stage pancreatic cancers (Nature Biomed. Eng. 2017).